Hanoi Ms. Mo, 31 years old, has had type 1 diabetes for more than 10 years. During pregnancy, she still ate and drank too little, leading to exhaustion.
On February 18, Dr. Le Ba Ngoc, Head of the Department of Internal Medicine, Tam Anh General Hospital, Hanoi, said that Ms. Mo was 5 weeks pregnant and in a state of exhaustion. BMI 18 - malnutrition, fasting blood sugar above 13 mmol/l (normal index is 5.3 mmol/l or less). Pregnant women need to change their diet to increase nutrition to ensure fetal development while still achieving the goal of controlling blood sugar. "This is a difficult problem for both doctors and patients," said Dr. Ngoc.
Dr. Ngoc coordinated with Dr. Vu Thi Thanh, Head of the Nutrition Department, to create a treatment plan for the patient, including a nutritional menu, medication, and exercise regimen. As the fetus grew, blood sugar levels changed constantly. Every day, Ms. Mo had to test her blood sugar 6 times before and after meals to adjust her medication dosage.
According to Dr. Ngoc, testing capillary blood sugar by pricking the fingertip is not feasible because pregnant women have to monitor their blood sugar daily. Dr. Ngoc advises pregnant women to use a continuous blood sugar monitor, which gives results on the machine without needing to prick the fingertip. This technology is more effective than the capillary blood sugar testing method.

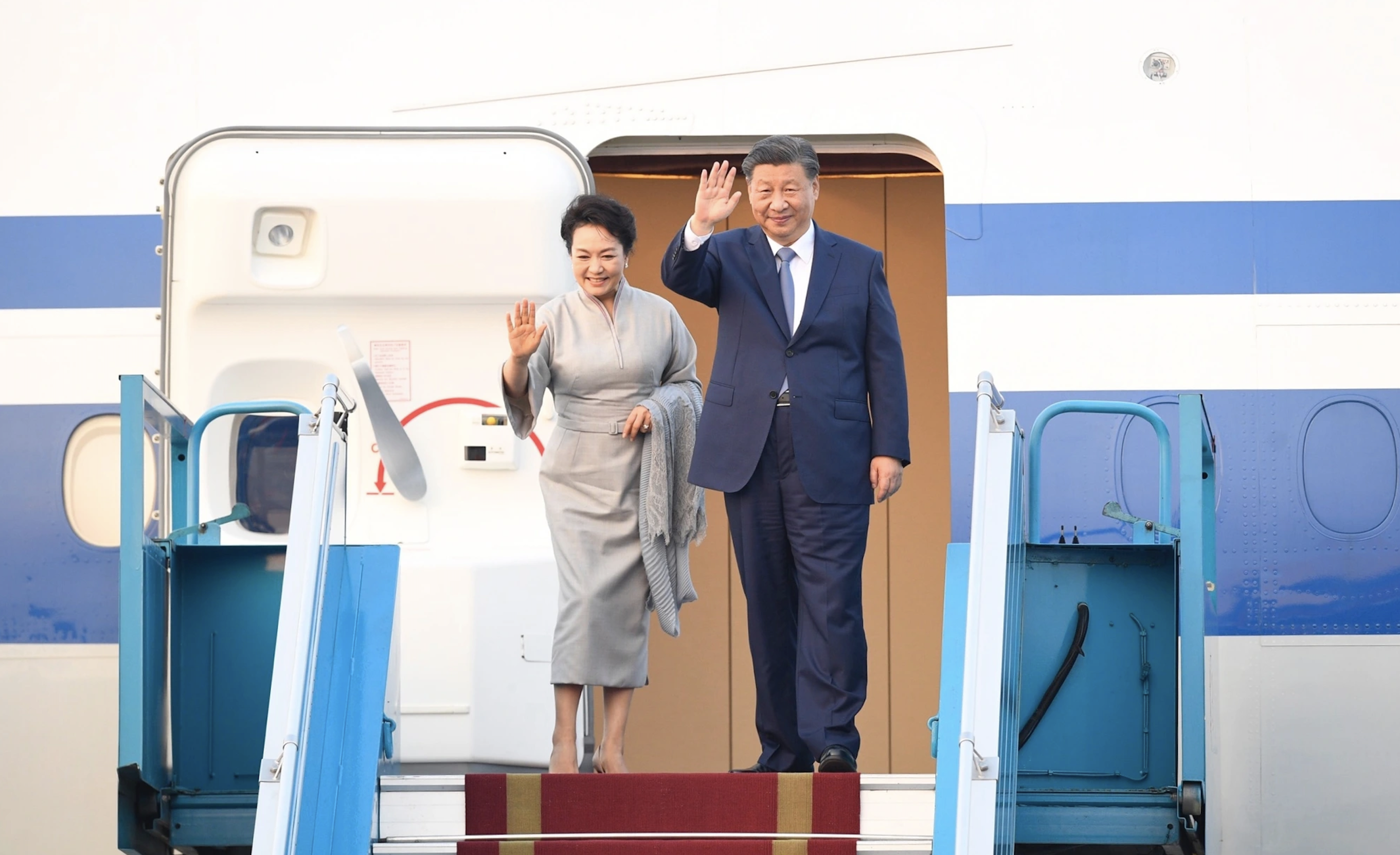
Doctor Ngoc consults on a patient's health condition. Photo: Provided by the hospital
After three follow-up visits, Ms. Mo followed the nutritional regimen and her weight and blood sugar levels reached the standard. She is currently 36 weeks pregnant, has gained 13 kg, her blood sugar index is stable, and the fetus weighs nearly 2.5 kg.
Diabetics, if not treated properly or with inadequate nutrition, can become obese or malnourished, leading to unstable blood sugar. Patients need to control their blood sugar before, during and after pregnancy.
Dr. Ngoc recommends that pregnant women with gestational diabetes should be advised on a plan to control blood sugar during labor and after birth. Newborns should be fed as soon as possible after birth to avoid the risk of hypoglycemia.
In the postpartum period, the insulin dose needs to be reduced compared to pregnancy to prevent hypoglycemia due to overdose. Pregnant women with type 1 diabetes continue to maintain insulin injections, monitor blood sugar to adjust the dose of medication. Patients who inject insulin do not affect the breastfeeding process, need to have a suitable diet, ensure the quality of milk for the baby, and at the same time help control blood sugar better.
Thanh Ba
* Patient's name has been changed
| Readers ask questions about obstetrics and gynecology here for doctors to answer |
Source link


![[Photo] Overcoming all difficulties, speeding up construction progress of Hoa Binh Hydropower Plant Expansion Project](https://vstatic.vietnam.vn/vietnam/resource/IMAGE/2025/4/12/bff04b551e98484c84d74c8faa3526e0)


![[Photo] Closing of the 11th Conference of the 13th Central Committee of the Communist Party of Vietnam](https://vstatic.vietnam.vn/vietnam/resource/IMAGE/2025/4/12/114b57fe6e9b4814a5ddfacf6dfe5b7f)
















![[Video] First time in Vietnam: Successful implantation of 3rd generation partial artificial heart](https://vstatic.vietnam.vn/vietnam/resource/IMAGE/2025/4/12/8817412224094c68ba2c744b7bd5cfea)


































































Comment (0)