Medical news August 25: Organ donation saves lives - Giving is forever
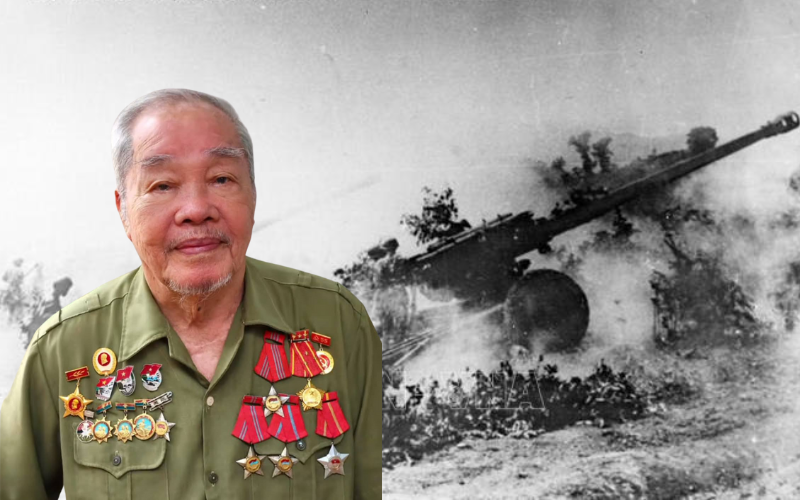
Overcoming the pain of losing a loved one, the family of a brain-dead patient in Hanoi agreed to donate organs to save the lives of many others.
Multi-organ transplant of brain-dead patient helps save many other patients
He passed away but still helped many other patients. The act of "overcoming the pain" of the family of the late patient N.D.Tr has lit up the hopes of many patients who are waiting for a miracle to save them. I would like to call him "The person who wrote the candle that was about to go out".
 |
| Overcoming the pain of losing a loved one, a brain-dead patient agreed to donate organs to save the lives of many others. |
At 11 p.m. on August 22, Xanh Pon General Hospital received a special case in critical condition. Patient N.D.Tr, 32 years old (Dong Anh, Hanoi) was admitted to the Emergency Department after a traffic accident. Although he had no previous medical history, the patient suffered a severe head injury and was transferred from Bac Thang Long Hospital to Xanh Pon Hospital.
The patient was admitted to the hospital in a deep coma, with many signs of serious trauma such as facial swelling, abdominal and pelvic hematoma. The patient was diagnosed with severe multiple injuries of unknown severity.
After performing the tests, the doctors decided to transfer the patient to the Operating Room - Department of Anesthesia and Resuscitation to perform the necessary interventions. However, the patient's condition continued to worsen and had to be transferred to the Resuscitation Room for further monitoring.
After 20 minutes, patient Tr. showed signs of brain death, the medical team conducted a clinical assessment according to regulations. Ms. Dinh Thi Thu Nga, Social Work Department, Xanh Pon General Hospital approached the family to encourage and share patient Tr.'s condition. Wiping away her tears and pain, patient Ng. TH's wife emotionally said in sobs, "My family and I are waiting for a miracle to come to him. If the miracle doesn't come, my family will donate his organs to help other patients."
She then turned away to wipe away the tears that were rolling down her tanned skin. So the miracle could not come to him, his parents, wife and two small children could not hold on to his life when the medical team had tried their best to save him. The team had performed the brain death assessment procedure and all three times had the same result. Mr. Tr had fallen into a state of brain death, his life was gradually closing.
In pain over the passing of their loved one, the patient's family still made a humane decision: to donate their loved one's organs to bring life to others.
Organs from brain-dead patients were coordinated for transplant to other patients. Mr. Tr. passed away but brought life to many people. His family's act of kindness will continue to write stories of everyday life - Giving is forever.
People with diabetes risk reduced life expectancy
Patients with type 2 diabetes who have cardiovascular, renal, and related metabolic diseases are at risk of significantly reduced life expectancy, from 6 to 15 years.
Professor, Dr. Tran Huu Dang, President of the Vietnam Endocrinology and Diabetes Association, said that currently there are about 537 million people in the world with type 2 diabetes, and the number of patients is estimated to increase to about 783 million by 2045.
Patients with type 2 diabetes have a higher risk of developing heart failure. Blood sugar control alone is not enough to protect the cardiovascular system. 44% of patients hospitalized for heart failure have type 2 diabetes. At the same time, up to 40% of patients with type 2 diabetes have chronic kidney disease.
According to Professor, Dr. Tran Huu Dang, cardiovascular, kidney and metabolic diseases, if coexisting in type 2 diabetes patients, will significantly reduce life expectancy.
Of these, type 2 diabetes patients have a life expectancy reduced by 6 years; type 2 diabetes patients with chronic kidney disease have a life expectancy reduced by 9 years; type 2 diabetes patients with myocardial infarction or stroke have a life expectancy reduced by 12 years. Notably, type 2 diabetes patients with myocardial infarction and stroke have a life expectancy reduced by 15 years.
Intensive glycemic control will reduce the occurrence of microvascular complications, and early intensive glycemic control will contribute to reducing cardiovascular events and mortality. Therefore, early, active and safe glycemic control is needed.
The goal of treating diabetic patients is not only to control blood sugar but also to prevent and treat complications, especially cardiovascular and renal complications.
Early use of appropriate drugs not only effectively controls blood sugar but also shows comprehensive protection of the cardiovascular and renal systems in patients with type 2 diabetes, helping to reduce cardiovascular complications, especially reducing the risk of cardiovascular death.
Burden of pneumococcal disease
At the scientific conference "Pneumococcal disease burden in adults", which recently took place in Ho Chi Minh City, experts said that according to research on the global disease burden, in 2021, the world had about 344 million cases of lower respiratory tract infections and 2.18 million deaths due to this condition.
Of these, pneumococcus is the cause of the highest rate of lower respiratory tract infections and deaths, with an estimated 97.9 million infections and 505,000 deaths. In Vietnam alone, the mortality rate due to pneumonia in 2021 was 18.2 cases per 100,000 people.
Although much progress has been made in reducing mortality from lower respiratory tract infections (LRTIs) and pneumococci, the burden remains high. The risk of invasive pneumococcal disease (IPD) in adults increases with age and in the presence of certain comorbidities.
According to the World Health Organization (WHO), an estimated 1.6 million people die each year from pneumococcal disease worldwide. Of these, 600,000-800,000 are adults, mainly due to pneumonia, meningitis and sepsis. More than 90% of these deaths occur in developing countries.
Associate Professor, Dr. Do Van Dung, former Head of the Faculty of Public Health, University of Medicine and Pharmacy, Ho Chi Minh City, shared that risk factors that increase the likelihood of contracting pneumococcal disease in adults include age (especially people over 65 years old) and weakened immune status.
People with chronic diseases such as cardiovascular disease, diabetes, and chronic liver disease also increase the risk of pneumococcal disease. In addition, lifestyle behaviors such as smoking and alcohol abuse increase the risk further, because smoking weakens the immune system and increases the risk of respiratory infections, while alcohol abuse can impair liver function and the immune system.
Many studies have shown that morbidity and mortality rates increase significantly with age and immune status of the patient. For example, patients with chronic cardiovascular disease are 3-7 times more likely to develop invasive pneumococcal disease (IPD) than healthy people; diabetic patients are 2-5 times more likely; chronic lung disease is 5-17 times more likely; cancer patients are 23-38 times more likely to develop IPD, etc.
The incidence of community-acquired pneumonia (CAP) increases with age and immune status of the patient, the mortality rate of invasive pneumococcal pneumonia varies from 6% to 20%.
Pneumococcal antibiotic resistance is also a global problem, leading to treatment failure and increased medical costs. In addition, the financial burden caused by pneumococcus is not small.
A 2004 study in the United States estimated that pneumococcal disease caused 4 million illnesses, 22,000 deaths, 445,000 hospitalizations, 774,000 emergency department visits, 5 million outpatient visits, and 4.1 million outpatient antibiotic prescriptions.
In addition, the economic burden of pneumococcal disease in adults over 50 years of age is approximately $3.7 billion in direct treatment costs and $1.8 billion in indirect costs each year. Pneumonia accounts for 22% of cases but accounts for 72% of treatment costs.
In Vietnam alone, the average cost of treatment for each patient with community-acquired pneumonia is 15-23 million VND (equivalent to 600-1,000 USD) and the average hospital stay is 6-13 days. Therefore, the role of timely disease prevention is very important.
In addition to non-specific preventive measures such as wearing masks, avoiding crowded places, limiting transmission routes... active prevention with vaccines is one of the most important solutions to deal with pneumococcal disease.
Source: https://baodautu.vn/tin-moi-y-te-ngay-258-hien-tang-cuu-nguoi---cho-di-la-con-mai-d223214.html


![[Photo] Summary of parade practice in preparation for the April 30th celebration](https://vstatic.vietnam.vn/vietnam/resource/IMAGE/2025/4/11/78cfee0f2cc045b387ff1a4362b5950f)
![[Photo] Prime Minister Pham Minh Chinh chairs meeting to discuss tax solutions for Vietnam's import and export goods](https://vstatic.vietnam.vn/vietnam/resource/IMAGE/2025/4/10/19b9ed81ca2940b79fb8a0b9ccef539a)
![[Photo] Phuc Tho mulberry season – Sweet fruit from green agriculture](https://vstatic.vietnam.vn/vietnam/resource/IMAGE/2025/4/10/1710a51d63c84a5a92de1b9b4caaf3e5)























































































Comment (0)