Ms. T. said she began experiencing numbness and weakness in both legs more than 9 months ago. After going to a hospital in the province, a doctor diagnosed her with venous insufficiency. She actively followed the prescription and practiced physical therapy, but her ability to walk and move gradually decreased.
On November 21, Meritorious Doctor - Master - Specialist Doctor 2 Chu Tan Si, Head of the Department of Neurosurgery, Tam Anh General Hospital, Ho Chi Minh City, said that Ms. T. was brought to the clinic by her family in a wheelchair in a state of very weak legs, unable to stand and unable to walk. The muscle strength of both legs was reduced by more than 70%, the muscles were flaccid, tendon reflexes were increased, there were signs of hypermobility and Babinski signs (signs indicating damage to the central nervous system).
MRI results showed a tumor about 3 cm in diameter in the thoracic spinal cord area D10 - D11 - D12, compressing and pushing the entire spinal cord from the right side to the left, deviated forward.
Risk of complete paralysis if not treated promptly
Dr. Tan Si stated that if this continues, Mrs. T. is at risk of being completely paralyzed. At that time, the tumor will grow larger, increasing pressure on the spinal cord and central nervous system, causing the patient's muscle strength to decline severely. This will lead to sphincter disorders, and inability to control bowel and bladder control.
The tumor is located in a dangerous position. Outside the tumor capsule, there are many nerve roots in the chest area. If the surgery is not done properly, it will damage the nerve roots. The patient was advised to have surgery guided by a robot using artificial intelligence (AI).
The advantage of this method is that the doctor can proactively plan the surgery and anticipate possible situations, helping to ensure success and safety for the patient.
The robot is capable of combining MRI, DTI, CT, DSA… to help doctors clearly see the entire thoracic spinal cord, nerve fiber bundles and tumors on the same image to choose the appropriate surgical path. In addition, the robot provides a simulated surgical feature on specialized software, helping doctors choose a safe approach to the tumor without damaging the nerves and spinal cord, minimizing risks to the patient.

Doctors during surgery on a patient with the assistance of an AI robot
Robot assisted spinal cord tumor surgery saves woman
The actual surgery is based on the surgical path established from the simulated surgery. The doctor opens the dura mater of the spinal canal and approaches the tumor. Then, the tumor capsule is opened and an ultrasonic suction cutter system is used to break and empty the tumor from the inside. Thereby, the volume of the tumor is reduced, creating favorable conditions for the dissection of the tumor capsule, minimizing the risk of damage to the spinal cord, nerve fiber bundles and surrounding healthy structures.
After removing the base of the tumor, the team proceeded to cut the stalk of the tumor, but bleeding began. This was predicted, so the doctors promptly used hemostasis techniques. After that, they completed the removal of the entire tumor for the patient.
The surgery lasted about 90 minutes, and the entire 3 cm meningeal tumor and the 1 cm tumor attachment on the meningeal membrane were removed. The surgery was minimally invasive, the patient did not lose vertebral bone, and did not need to have screws placed.
After 2 days of surgery, Mrs. T.'s health recovered. The severe symptoms, numbness in both legs and muscle strength improved significantly. Mrs. T. can walk more easily and climb stairs. It is expected that Mrs. T. can be discharged in the next 3 days. If she actively practices physical therapy for a while longer, her legs will likely recover completely.
Dr. Tan Si said that the removed spinal cord tumor was benign and had no genetic factors. However, Ms. T. still needs to be re-examined after 3 months to assess the recovery of the spinal cord and nerve conduction bundles.
"People with symptoms of heavy legs, numb legs, difficulty walking, sensory disturbances, etc. should be promptly examined by a neurologist. Patients need to be scanned and have necessary tests done to correctly identify the disease, eliminate physical damage, and then treat functional damage. Avoid misdiagnosis that causes prolonged damage and is dangerous for the patient," Dr. Tan Si advised.
Quick view 12:00 on November 21: Panorama news
Source link


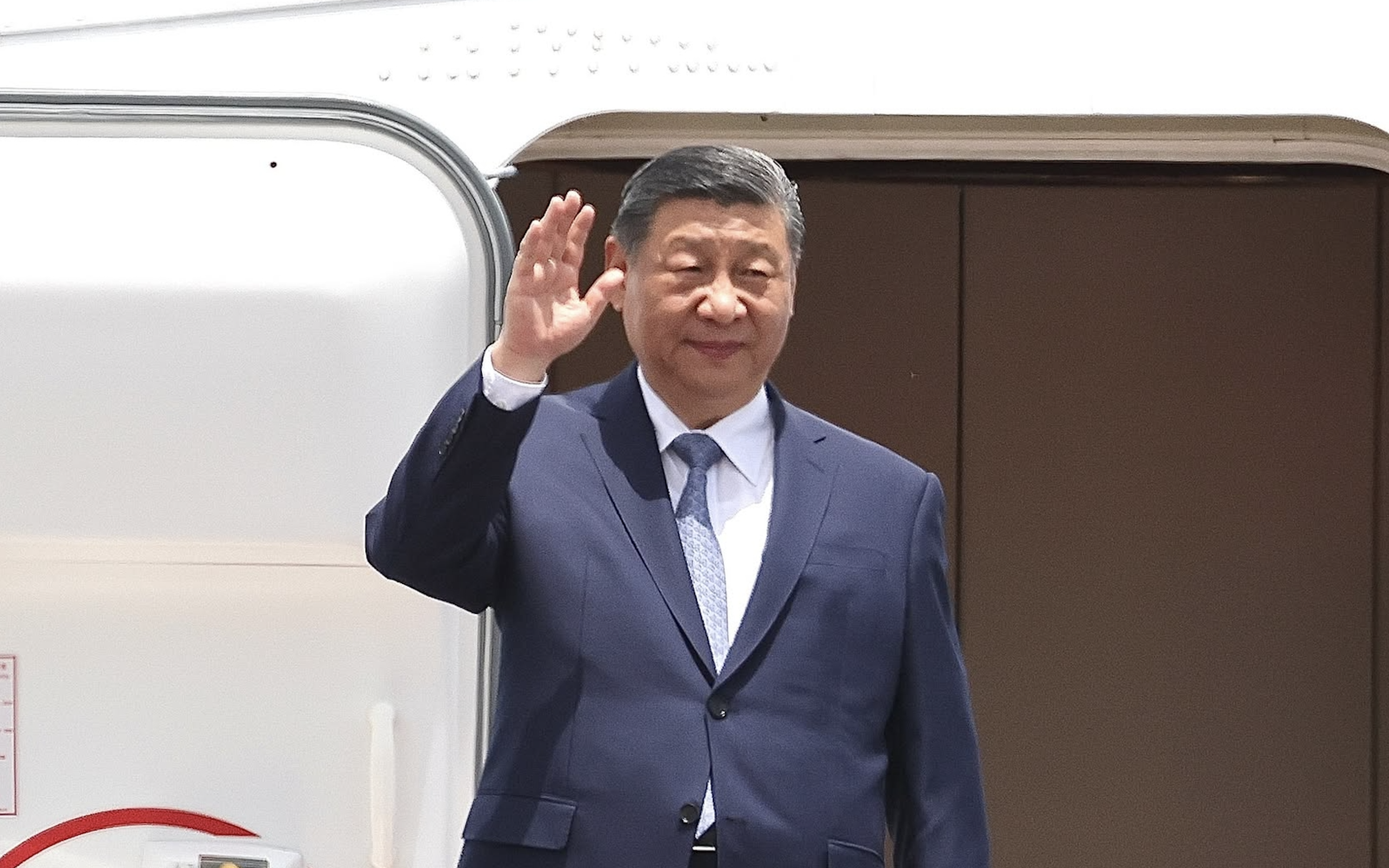
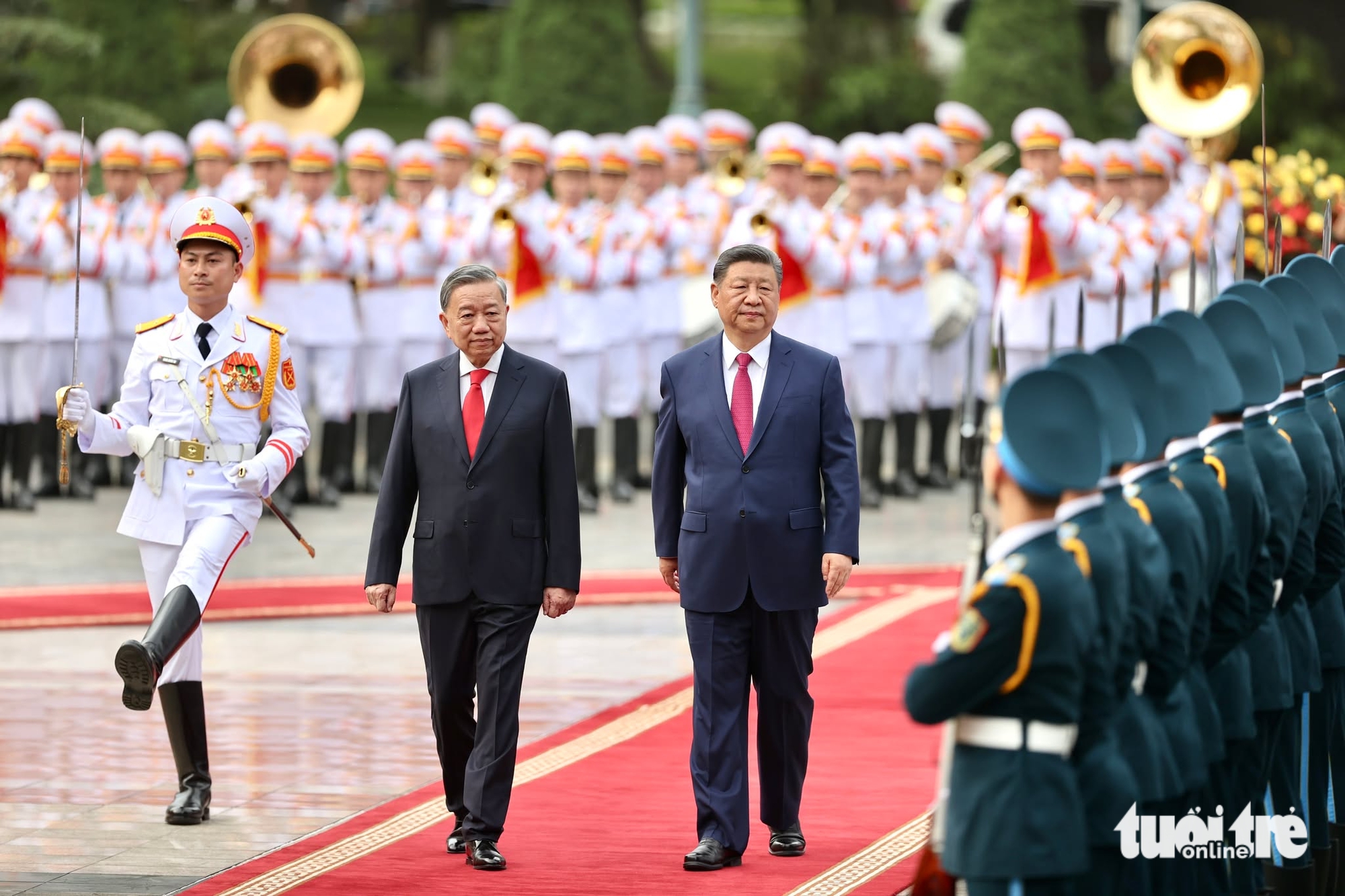
![[Photo] Reception to welcome General Secretary and President of China Xi Jinping](https://vstatic.vietnam.vn/vietnam/resource/IMAGE/2025/4/14/9afa04a20e6441ca971f6f6b0c904ec2)
![[Photo] Prime Minister Pham Minh Chinh meets with General Secretary and President of China Xi Jinping](https://vstatic.vietnam.vn/vietnam/resource/IMAGE/2025/4/14/893f1141468a49e29fb42607a670b174)
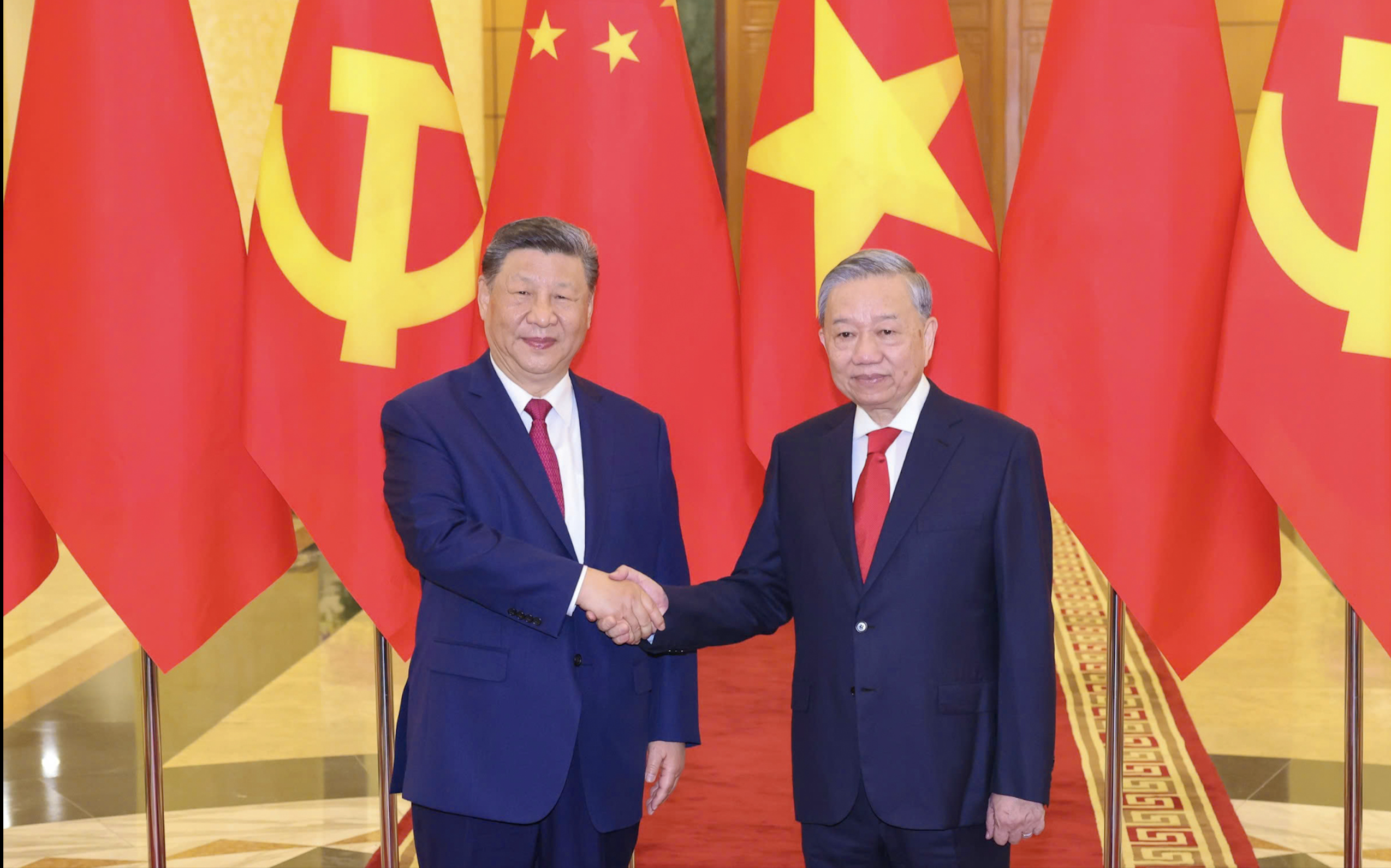
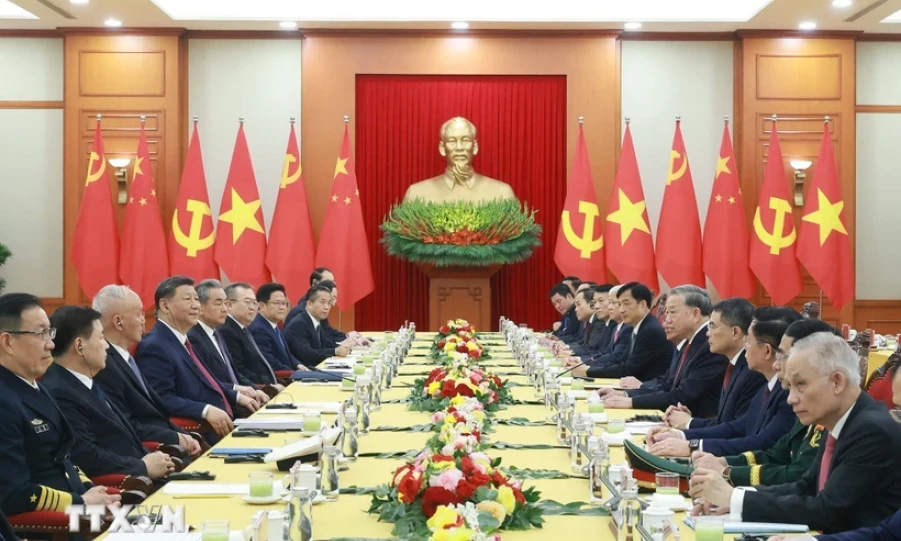
![[Photo] General Secretary To Lam holds talks with General Secretary and President of China Xi Jinping](https://vstatic.vietnam.vn/vietnam/resource/IMAGE/2025/4/14/b3d07714dc6b4831833b48e0385d75c1)

![[Photo] National Assembly Chairman Tran Thanh Man meets with General Secretary and President of China Xi Jinping](https://vstatic.vietnam.vn/vietnam/resource/IMAGE/2025/4/14/4e8fab54da744230b54598eff0070485)








































































Comment (0)