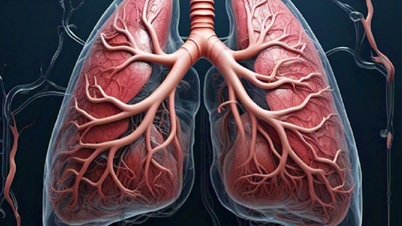
A spike in rare autoimmune disease cases during the COVID-19 outbreak in the UK has led to the discovery of a new syndrome. It is a new autoimmune syndrome linked to COVID-19 that can cause life-threatening lung disease.
The syndrome — which scientists call “MDA5 Autoimmune Interstitial Pneumonitis Concurrent with COVID-19,” or MIP-C for short — is a rare, severe condition in which the immune system mistakenly attacks the body. In the worst cases, the lungs become so scarred and stiff that the only way to save them is with a whole lung transplant.

Scientists say they have discovered an autoimmune syndrome that may be linked to COVID-19. (Photo: Christoph Burgstedt/ Science Photo Library)
However, only a small fraction of cases involve the lungs. “Two-thirds of the cases we studied did not have lung disease,” said Dr Dennis McGonagle, a rheumatologist at the University of Leeds in the UK who first began studying models of the new disease. “But we found that eight cases progressed rapidly and died despite all the high-tech therapies we could give them.”
In total, McGonagle and his colleagues have identified 60 cases of the syndrome so far. They published their research in the May issue of the journal eBioMedicine.
McGonagle says the disease looks similar to a known condition called MDA5 dermatomyositis, which mostly affects women of Asian descent. Patients have joint pain, muscle inflammation, and skin rashes, and in two-thirds of cases, life-threatening lung scarring. MDA5 dermatomyositis occurs when the immune system attacks one of its own proteins: a protein called MDA5 that normally helps detect RNA viruses. These viruses include those that cause influenza, Ebola, and COVID-19.
McGonagle said the new research suggests that exposure to coronavirus RNA, a Covid-19 vaccine, or both can sometimes trigger the production of anti-MDA5 antibodies.
Normally, MDA5 is activated when it senses viral RNA in a cell and prompts the body to make antibodies to fight the virus. But in people with MIP-C, this immune response goes awry. McGonagle suggests that either the body mistakes the MDA5 protein as a foreign protein and attacks it, or the RNA triggers such a strong immune response that the body’s own proteins, including MDA5, become targets of immune attack.
The researchers found that IFIH1 activation was accompanied by high levels of an inflammatory protein called interleukin-15 (IL-15). IL-15 activates a class of immune cells that normally kill infected cells but can sometimes attack the body's own cells.
Source


![[Photo] President Luong Cuong presents the 40-year Party membership badge to Chief of the Office of the President Le Khanh Hai](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/5/19/a22bc55dd7bf4a2ab7e3958d32282c15)



![[Photo] Close-up of Tang Long Bridge, Thu Duc City after repairing rutting](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/5/19/086736d9d11f43198f5bd8d78df9bd41)
![[Photo] Panorama of the Opening Ceremony of the 43rd Nhan Dan Newspaper National Table Tennis Championship](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/5/19/5e22950340b941309280448198bcf1d9)























![[Photo] General Secretary To Lam attends the conference to review 10 years of implementing Directive No. 05 of the Politburo and evaluate the results of implementing Regulation No. 09 of the Central Public Security Party Committee.](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/5/19/2f44458c655a4403acd7929dbbfa5039)


























































![[VIDEO] - Enhancing the value of Quang Nam OCOP products through trade connections](https://vphoto.vietnam.vn/thumb/402x226/vietnam/resource/IMAGE/2025/5/17/5be5b5fff1f14914986fad159097a677)



Comment (0)