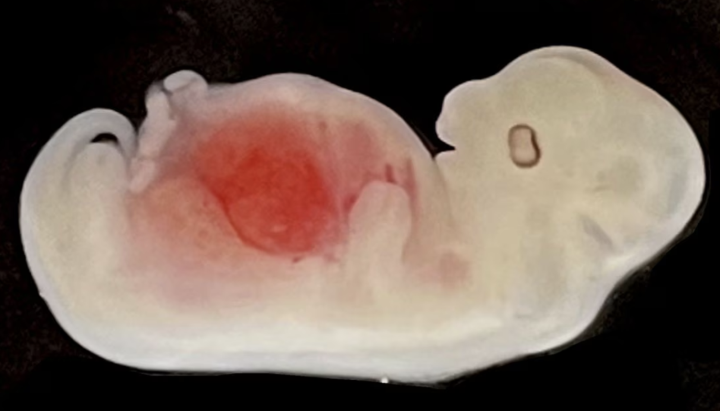
A 28-day-old pig embryo has a replica of a human kidney. (Photo: GIBH)
This is a historic image. A team of researchers in China has successfully created, for the first time, replicas of human organs in another animal species.
Experiments conducted with cloned kidneys in pig embryos represent a step toward the dream of using other mammals as organ sources for transplantation. However, these "hybrid" organs still raise significant ethical concerns.
Researchers at the Guangzhou Institute of Biomedical Sciences have reprogrammed adult human cells to restore their ability to form any organ or tissue in the body. The research team introduced these multipotent human cells into pig embryos, which had been genetically modified beforehand so they wouldn't develop into pig kidneys. The human cells filled that gap and created a "primitive" kidney, an intermediate stage of the renal system called a mesonephros.
The research team implanted a total of 1,820 embryos into 13 sows, then terminated the pregnancies on days 25 and 28 (approximately one-quarter of the normal gestation period for pigs) for evaluation. The results showed that 5 selected embryos had normally functioning kidneys during development, with ureters beginning to form to connect to the bladder. These kidneys contained 50-60% human cells.
The research was led by Chinese scientist Liangxue Lai, but the idea was initiated by a team led by Spanish researcher Juan Carlos Izpisua. In 2017, Izpisua announced the creation of human-pig embryos with a ratio of human cells to pig cells of 1 in 100,000. These pioneering experiments were conducted at the University of Murcia (Spain) and at two Murcian farms, despite intense debate by a committee of experts at the Carlos III Institute of Health. Ultimately, the committee allowed the experiments to proceed despite “the inherent biological risks in creating a human-pig hybrid,” but on the condition that no animals with human cells could reproduce.
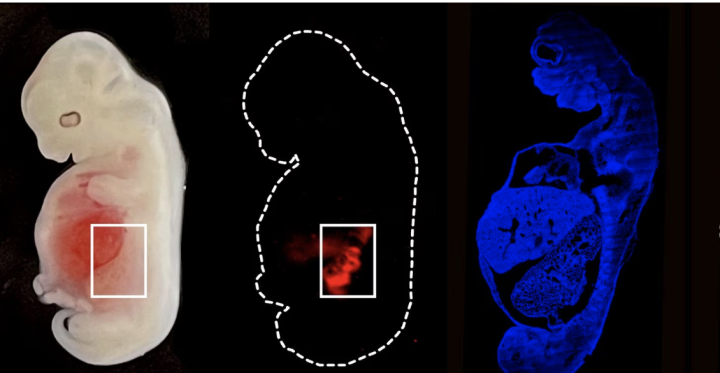
A 28-day-old pig embryo growing a kidney contains half human cells. (Photo: GIBH)
Izpisua welcomed the new research, in which he was not involved. The researcher, who is also the director of the San Diego Institute of Science at Altos National Laboratory in the U.S., said: “They’ve taken it a step further and shown that cells can be organized in space and create organized tissue structures.”
Izpisua commented: “It’s still not possible to develop mature human-like organs in pigs, but this research brings us one step closer. It’s a big step forward.”
According to official data, around 150,000 organs are transplanted worldwide each year, but in the US alone, there are 100,000 people on the organ transplant waiting list, and 17 of them die every day.
Liangxue Lai and the team of Spanish researcher Miguel Angel Esteban are currently working towards the goal of obtaining mature kidneys, although they still have to overcome technical and ethical hurdles. One of the red lines is preventing human cells from escaping the kidney and integrating into the pig's brain or its gonads (testes or ovaries).
"The question is whether it's ethical to allow pigs to be born with mature, cloned kidneys. It will all depend on the extent to which human cells contribute to the pig's other tissues," Esteban said.
His research, published on September 7 in the journal Cell Stem Cell, shows that “very few” human cells are dispersed throughout the brain and spinal cord of pig embryos. The Spanish doctor stated: “To eliminate any ethical concerns, we are further modifying the human cells so that they cannot penetrate the pig’s central nervous system in any way.”
In 2020, a research team from the University of Minnesota successfully created human endothelium (the inner layer of blood vessels) in pig embryos.
A year later, the same team, led by Mary Garry and Daniel Garry, created 27-day-old pig embryos with cloned muscles.

Spanish doctor Miguel Ángel Esteban (right) and his Chinese colleague Liangxue Lai at the Guangzhou Institute of Biomedical Sciences and Health. (Photo: GIBH)
With the new trial in China, nephrologist Rafael Matesanz, founder and former director of the National Transplant Foundation in Spain, noted that this is the first time a human organ has been created inside another animal. The nephrologist stated: “ Conceptually, this is a very important and significant step, but it is not the prelude to kidney production .”
Matesanz was one of the members of the committee authorizing Izpisua's experiments in Murcia. In his opinion, it was "doubted" that an experiment like the one being conducted in Guangzhou would be approved in Europe, given the possibility that some human cells could invade the brain of pig embryos, which has indeed happened.
" The main risk is that the cells will travel to the central nervous system and create a human-pig hybrid. Or that they will travel to the reproductive system ," he warned.
The founder of the National Transplant Organization believes that “a far more promising path” is to create genetically modified pigs so that pig organs do not cause rejection in humans after transplantation. On September 25, 2021, a team of surgeons at New York University successfully transplanted a pig kidney into a brain-dead woman. On January 7, 2022, following surgery at the University of Maryland Medical Center, American citizen David Bennett became the first person to have a beating pig heart in his chest. Bennett died two months later from heart failure, but showed no obvious signs of organ rejection, despite the heart being infected with swine flu.
Spanish chemist Marc Güell is one of the founders of eGenesis, a US company that modifies pig DNA to create pig organs for human transplantation. Güell also welcomed these new results: “ It could help to better understand the current limits of chimerism between species .”
Dr. Josep Maria Campistol, a nephrologist and General Director of the Clínic de Barcelona, emphasized all the prospects opened up by pig-human embryos. He said: “ They could be an inexhaustible source of organs, and offer the possibility of creating specific, personalized human body parts for certain patients .”
(Source: News Report)
Source





![[Photo] Prime Minister Pham Minh Chinh working with the Vietnam Academy of Science and Technology](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2026/02/23/1771832245861_image-2-6431-jpg.webp)
![[Photo] General Secretary To Lam meets with and extends New Year greetings to the Central Party Office.](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2026/02/23/1771822040571_a1-bnd-6844-9653-jpg.webp)
![[Photo] Nhan Dan Newspaper's New Year's gathering in the year of the Horse 2026](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2026/02/23/1771825639110_gap-mat-dau-xuan1-8272-jpg.webp)








































































































Comment (0)