Liver biopsy helps diagnose and evaluate lesions of unknown cause, classifying them as benign or malignant.
Dr. Vu Truong Khanh, Head of the Department of Gastroenterology, Tam Anh General Hospital, Hanoi, said that liver biopsy is performed to diagnose liver problems that cannot accurately determine the cause or whether the lesion is benign or malignant by blood tests, imaging diagnosis...
Liver biopsy helps determine the severity of the disease (stage) and the rate of progression of the disease (classification), thereby developing a treatment plan based on the type, stage, grade, and predicted treatment outcome (prognosis). Patients can have a liver biopsy when there is a tumor in the liver.
According to Dr. Khanh, non-invasive methods such as ultrasound and liver elasticity measurement have made many advances, but biopsy is still the "gold" standard for diagnosing and distinguishing many liver diseases such as fatty liver disease, chronic hepatitis, cirrhosis, liver cancer...
This method helps the doctor isolate specific causes or types of diseases such as alcoholic liver disease, autoimmune hepatitis, hepatocellular carcinoma, Hodgkin lymphoma, primary biliary cholangitis, toxic hepatitis, viral hepatitis B or C.
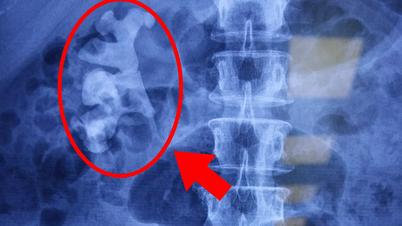
There are many indications for liver biopsy, which fall into three main categories:
Diagnosis: Liver biopsy is important when diagnosis is difficult. For example, differentiating autoimmune hepatitis from nonalcoholic steatohepatitis in an obese patient with abnormal liver function tests and positive autoimmune serologies.
Liver biopsy is useful when there are overlapping syndromes such as autoimmune hepatitis and primary biliary cholangitis. Liver biopsy is also used to evaluate abnormal liver function tests shortly after liver transplantation. In cases where it is not possible to differentiate cholangiocarcinoma from hepatocellular carcinoma, liver biopsy may be performed.
Prognosis: Liver biopsy can be used as a prognostic tool for several diseases, including nonalcoholic fatty liver disease with progression to cirrhosis, hemochromatosis, and viral hepatitis.
Treatment: Liver biopsy is important for people with autoimmune hepatitis who are being treated with steroids and immunomodulators.

Dr. Vu Truong Khanh examines a patient. Photo: Provided by the hospital
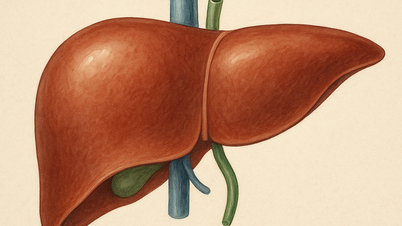
Currently, there are three types of liver biopsy commonly used today: percutaneous biopsy under ultrasound guidance. The biopsy process only takes a few tens of seconds because the needle moves quickly in and out of the liver.
Intravenous biopsy : The doctor applies a numbing agent to the side of the patient’s neck. Then, a small incision is made, a flexible plastic tube is inserted into the neck vein and into the vein above the liver. The doctor passes a biopsy needle through the tube to remove one or more liver samples. This procedure can be performed safely even if the liver’s clotting function is impaired.
During a laparoscopic biopsy , the patient is given general anesthesia. The doctor makes one or more small incisions in the patient's abdomen, inserting special instruments through the incisions to take tissue samples with the help of a small camera. The incisions are closed with stitches after the instruments and liver tissue samples are removed. This method is rarely performed alone, but is often performed in combination with a liver biopsy during laparoscopic surgery.
Dr. Khanh added that after taking the sample, the liver tissue is evaluated by pathologists. Based on the size and shape of the liver cells and other factors, the biopsy can indicate the cause of the liver damage, whether it is benign or malignant.
Emerald
| Readers ask questions about digestive diseases here for doctors to answer |
Source link


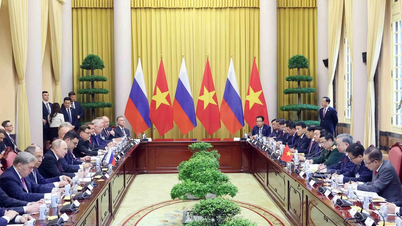
![[Photo] General Secretary To Lam begins official visit to Russia and attends the 80th Anniversary of Victory over Fascism](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/5/8/5d2566d7f67d4a1e9b88bc677831ec9d)
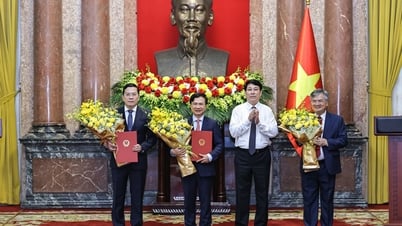
![[Photo] President Luong Cuong presents the decision to appoint Deputy Head of the Office of the President](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/5/8/501f8ee192f3476ab9f7579c57b423ad)
![[Photo] National Assembly Chairman Tran Thanh Man chairs the meeting of the Subcommittee on Documents of the First National Assembly Party Congress](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/5/8/72b19a73d94a4affab411fd8c87f4f8d)
![[Photo] Prime Minister Pham Minh Chinh meets with the Policy Advisory Council on Private Economic Development](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/5/8/387da60b85cc489ab2aed8442fc3b14a)
![[Photo] General Secretary concludes visit to Azerbaijan, departs for visit to Russian Federation](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/5/8/7a135ad280314b66917ad278ce0e26fa)




















































![[Photo] Prime Minister Pham Minh Chinh talks on the phone with Singaporean Prime Minister Lawrence Wong](https://vphoto.vietnam.vn/thumb/402x226/vietnam/resource/IMAGE/2025/5/8/e2eab082d9bc4fc4a360b28fa0ab94de)
































Comment (0)