With the ability to differentiate into many different cell types, stem cells are used in the treatment of many diseases and play an important role in medical research and drug development.
Stem cells play a fundamental role in the development of new drugs. Today, most new drugs must undergo animal testing (in vivo testing) before they can be used in humans. However, even if a drug is completely suitable in animals, it cannot be guaranteed that it will be completely safe for use in humans. The ideal solution to the problem of drug side effects is to test the drug on human cells (in vitro testing) before it goes into human clinical trials.
Many studies have demonstrated that stem cells are effective tools for drug research and development. One study (2023) showed that stem cells provide an ideal in vitro testing platform for pharmacological research. They allow the identification of new molecular targets, the evaluation of pharmacological effects of compounds, and the prediction of clinical efficacy. Typical examples include the creation of cancer models from patient stem cells to evaluate the effectiveness of immunotherapies.
In addition to replacing lost or damaged tissue, stem cells can also help speed up drug research and screening. By using stem cells to simulate disease at the cellular level, scientists can better understand disease mechanisms and effectively screen compounds with drug potential.
According to the California Institute for Regenerative Medicine (CIRM), the application of stem cell technologies after clarifying disease mechanisms will shorten the time and cost of drug development. Stem cell technology is expected to significantly improve the ability of pharmaceutical companies to screen new drugs for side effects much earlier in the development process, significantly reducing the time it takes to develop a new drug.
Many countries in the world such as the US, Canada, Germany, Japan, China, etc. have applied stem cell technology to successfully develop new drugs. Currently, the most popular are applied pluripotent stem cell technology (iPS) and somatic cell nuclear transfer technology (SCNT). Pluripotent stem cells created through iPS cell technology and SCNT will create cell lines with genetic characteristics identical to the person who donated the cells.
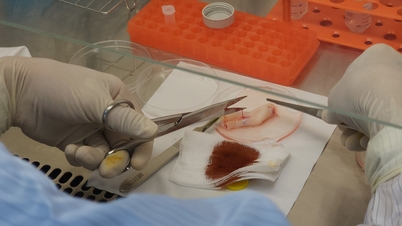
One example is the research process for producing anti-inflammatory drugs for Parkinson's patients. The drug research process begins by taking a small sample of skin cells from a Parkinson's patient. Scientists will culture this sample of cells under special conditions to turn them into nerve cells identical to the damaged cells in the patient's brain. After a period of monitoring, these new cells will accurately reproduce the Parkinson's disease process in the culture dish. Researchers will observe in detail the changes that occur inside the cells when the disease starts. Thereby, developing methods for screening drugs earlier, helping to prevent, slow down, stop or even reverse the progression of Parkinson's disease.
Stem cells are also used to evaluate the safety and potential risks of new drugs. According to Dr. Bruce Conklin, senior researcher at the Gladstone Institute of Cardiovascular Disease, drug screening using pluripotent stem cells is an effective method to detect toxic side effects. Accordingly, stem cells will be cultured into mature cell types such as heart cells, liver cells or brain cells, then exposed to new drugs and/or potential environmental hazards to record possible side effects. For example, using neural stem cells to study Alzheimer's disease and screen beta-amyloid inhibitors.
In reality, the drug testing process takes years and costs millions of dollars. In the United States, a new drug must go through four stages before it can be marketed: discovery and development, preclinical research, clinical trials, and FDA review. In addition, the average time it takes for a drug to go through the various stages of development and receive approval from the European Medicines Agency (EMA) or the U.S. Food and Drug Administration (FDA) is 10 years.
In the long term, stem cells open up new avenues for personalized drug therapy. By creating individual disease models using the patient’s own stem cells, scientists and healthcare providers will be able to predict how each patient will respond to each drug, increasing the success rate of treatment and shortening recovery time.
Source: https://baodautu.vn/phat-trien-thuoc-moi-tu-cong-nghe-te-bao-goc-d227540.html



![[Photo] Close-up of heavy damage at the school located on the banks of the Ban Thach River](/_next/image?url=https%3A%2F%2Fvphoto.vietnam.vn%2Fthumb%2F1200x675%2Fvietnam%2Fresource%2FIMAGE%2F2025%2F11%2F26%2F1764152130492_ndo_bl_img-8188-8805-jpg.webp&w=3840&q=75)







































































![[Photo] Opening of the 28th Session of the Hanoi People's Council](https://vphoto.vietnam.vn/thumb/402x226/vietnam/resource/IMAGE/2025/11/26/1764155991133_image.jpeg)































Comment (0)