Hanoi Mr. Duong, 42 years old, had dull abdominal pain and fever. The doctor diagnosed him with a neuroendocrine tumor in a rare location, with only about 150 cases recorded in world medical literature.
The results of endoscopic ultrasound and MRI of the patient's abdomen showed a tumor protruding into the duodenum at the papilla of Vater (the last section of the bile duct and pancreatic duct that flows into the duodenum). The tumor was about 2x2 cm in size, with an ulcerated, bleeding surface.
On September 27, Dr. Dao Tran Tien, Deputy Head of the Department of Gastroenterology, Tam Anh General Hospital, Hanoi, diagnosed a carcinoid neuroendocrine tumor in the duodenum ampulla, not yet invading the biliary tract or pancreas, requiring early intervention to avoid complications.
"Neuroendocrine tumors are mostly found in the digestive tract such as the stomach, small intestine, colon, rectum, appendix, pancreas, but are rare in the ampulla of Vater," said Dr. Tien, adding that to date there have only been about 150 reported cases worldwide.
The incidence is about 0.3-1% of all cases of neuroendocrine tumors in the digestive tract and less than 2% of all digestive tract cancers. In Vietnam, studies have recorded similar cases as quite rare.
According to Dr. Tien, the ampulla of Vater has a complex anatomical structure, with many large blood vessels. If the duodenum is opened, the patient is likely to have complications such as pancreatic fistula, infection, scarring from the open surgery, and a long hospital stay and recovery time. The patient's total pancreaticoduodenal resection may have long-term effects on health and reduce quality of life. The team decided to perform endoscopic retrograde cholangiopancreatography to remove the ampulla of Vater tumor, helping to preserve the digestive tract and reduce the risk of complications.

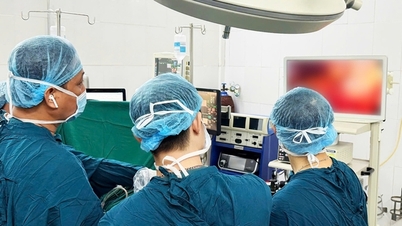
Doctor Tien (right) and the endoscopic intervention team performed a tumor removal procedure on the patient. Photo: Provided by the hospital
With the support of the X-ray fluorescence screen (C-Arm), the doctor completely cut the tumor. The cut site was closed with a specialized clip, helping the wound heal quickly, avoiding complications. The doctor placed a biliary stent and a pancreatic stent to ensure bile duct recirculation, preventing complications such as edema, secondary biliary obstruction, and acute pancreatitis.
After surgery, the patient's health was stable, he could eat soft foods, and had normal activities. He was discharged two days later. Pathology results showed that the tumor had a high degree of differentiation (ie low malignancy), and had been completely cured. The patient only needed to be monitored and returned for check-ups as scheduled without having to undergo adjuvant or chemical treatment.
Dr. Tien added that most ampullary tumors are malignant. If not detected and treated early, cancer cells can metastasize to other organs in the body, making treatment difficult. In addition, cancerous tissue can cause ampullary blockage, bile and pancreatic juice cannot flow into the small intestine to digest food, causing bile obstruction, biliary tract infection, acute pancreatitis, biliary peritonitis, and death.
Neuroendocrine tumors are common in people aged 50-60, and women are more likely to be affected than men. The cause of the disease is currently unknown. Factors that increase the likelihood of tumor development include people with multiple endocrine neoplasia type 1 (MEN1), neurofibromatosis type 1, and Von Hippel-Lindau (VHL) syndrome.
Gastrointestinal neuroendocrine tumors progress silently, without typical symptoms in the early stages. In later stages, clinical symptoms manifest differently depending on the location of the tumor, easily confusing with many other digestive diseases. The disease can only be completely cured in the early stages.
According to Dr. Tien, primary tumors are often small, so CT or MRI scans are only 33% sensitive in diagnosis. To assess the detailed morphological characteristics of the tumor, doctors need the support of an endoscopic ultrasound machine, which helps detect deep lesions under the thin layers of the digestive tract wall as well as the surrounding lymph nodes and blood vessels. From there, the regional lymph nodes and the extent of the lesion's invasion can be assessed to come up with an appropriate treatment plan.
Doctors advise people with unusual symptoms such as diarrhea, nausea and vomiting, abdominal pain, red skin, constipation, to go see a doctor for early diagnosis.
Trinh Mai
* Character names have been changed
| Readers ask questions about digestive diseases here for doctors to answer |
Source link








































































































Comment (0)