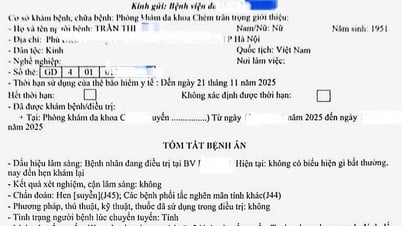
On June 26, Dr. Vu Duc Cong, Men's Health Center (HCMC), said that the patient shared that although he had sex regularly 2-4 times/week, after 2 years of marriage, he still had no "sweet results". That prompted him to decide to go to a urologist.
When holding the semen analysis results, Mr. H. could not believe that there was not a single sperm in the semen sample. Because he thought that if his "little guy" was still erect and capable of normal intercourse, his fertility would be good.

Having sex regularly 2-4 times/week but after 2 years of marriage still no "sweet results"
"The patient was shocked when the doctor informed him that his two testicles had shrunk, the size of a baby's testicles," Dr. Cong shared.
Doctor Cong said that the results of the screening tests showed that the patient's testicles were quite severely damaged, so the possibility of finding sperm through natural ejaculation was very low. The patient was assigned to undergo microsurgery to find sperm (MicroTESE) to extract sperm from the undamaged seminiferous tubules.
"Before the surgery, Mr. H. was given medication by the doctor to increase the chance of finding sperm for 6 months before the surgery. Finally, thanks to their perseverance, luck smiled on Mr. H. and his wife after 2 hours of surgery. The number of sperm was enough for in vitro fertilization," said Dr. Cong.
What is the normal volume of a testicle?
According to Dr. Cong, statistics in Vietnam show that normal testicular volume is from 12-25 ml. Testicular volume under 12 ml is considered small testicle. Because the testicle is oval in shape, it will be measured with a special ruler called Prader.
The measuring rods are egg-shaped plastic rods of different sizes corresponding to 1 - 2 - 3 - 5 - 6 - 8 - 10 - 12 - 15 - 20 - 25 - 30 ml. With this ruler, the doctor can measure the volume of the testicles with the most specific and accurate numbers.
According to Mr. H., his testicles used to be quite large. But after going through a 2-week orchitis, he noticed that his testicles were getting smaller. Apart from the change in size, testicular atrophy does not cause discomfort to the patient, so over time, Mr. H. forgot about this symptom.
Orchitis causes the internal structures of the testicles to be destroyed. Therefore, after the inflammatory stage, the testicles will usually atrophy.
Causes of testicular atrophy
Doctor Cong said that in addition to orchitis, there are many other causes of testicular atrophy such as:
Genetic diseases : These are cases where the testicles do not change in size from childhood to adulthood. In addition to the manifestations in the testicles, genetic abnormalities also cause puberty disorders, making men, despite their age, still not mature.
Mumps orchitis : Mumps orchitis has a similar course. However, the degree of testicular destruction caused by the mumps virus is higher than that of common bacteria, especially mumps causes the disappearance of spermatocytes, causing severe destruction of testicular tissue. Therefore, testicular atrophy after mumps is a sign of a high risk of infertility.
Varicocele : This is a fairly common disease in men. If not examined and treated promptly, it can cause damage and atrophy of the testicles. However, the disease progresses silently and sometimes does not cause any discomfort to the patient. Therefore, when men see their testicles shrink, they should screen for this cause.
Reproductive endocrine system : Testicular atrophy with decreased libido, erectile dysfunction, and premature ejaculation are signs that the male endocrine system is abnormal. Therefore, reproductive endocrine testing is necessary for these subjects.
"There are many causes of testicular atrophy, and each cause has a different treatment. For patients with testicular atrophy but stable sperm quality, the doctor will prescribe oral medication. On the contrary, in cases of testicular atrophy where there is no sperm in the semen sample, it is necessary to assess the extent of testicular damage before deciding on surgical intervention," said Dr. Cong.
Source link


![[Photo] Panorama of the Opening Ceremony of the 43rd Nhan Dan Newspaper National Table Tennis Championship](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/5/19/5e22950340b941309280448198bcf1d9)
![[Photo] President Luong Cuong presents the 40-year Party membership badge to Chief of the Office of the President Le Khanh Hai](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/5/19/a22bc55dd7bf4a2ab7e3958d32282c15)
![[Photo] Close-up of Tang Long Bridge, Thu Duc City after repairing rutting](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/5/19/086736d9d11f43198f5bd8d78df9bd41)

![[Photo] General Secretary To Lam attends the conference to review 10 years of implementing Directive No. 05 of the Politburo and evaluate the results of implementing Regulation No. 09 of the Central Public Security Party Committee.](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/5/19/2f44458c655a4403acd7929dbbfa5039)



























![[Photo] Prime Minister Pham Minh Chinh inspects the progress of the National Exhibition and Fair Center project](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/5/19/35189ac8807140d897ad2b7d2583fbae)






















































![[VIDEO] - Enhancing the value of Quang Nam OCOP products through trade connections](https://vphoto.vietnam.vn/thumb/402x226/vietnam/resource/IMAGE/2025/5/17/5be5b5fff1f14914986fad159097a677)





Comment (0)