While many countries still find first-generation antibiotics effective, Vietnam has had to resort to third and fourth-generation antibiotics. This is due to the indiscriminate buying and use of antibiotics in treatment, leading to an increasingly alarming rate of antibiotic resistance.
 |
Healthcare workers care for a patient who has developed drug resistance. |
Critically ill due to self-medication with antibiotics.
The University Medical Center of Ho Chi Minh City recently admitted and treated patient D.VN (70 years old, residing in Ben Tre province) who was hospitalized locally due to shortness of breath for two weeks. Prior to this, he had self-medicated with antibiotics but his condition did not improve. His family then transferred him to the University Medical Center of Ho Chi Minh City in a critical condition requiring mechanical ventilation and intubation. He was diagnosed with pneumonia caused by Klebsiella pneumoniae (one of the gram-negative bacteria with a high rate of antibiotic resistance).
Mr. N. was treated with colistin (a last-resort antibiotic for multidrug-resistant Gram-negative bacteria). Subsequent sputum cultures showed the persistence of multidrug-resistant Klebsiella pneumoniae (only sensitive to one group of aminoglycoside antibiotics – a potent group but with nephrotoxicity and vestibular toxicity, a narrow therapeutic range, and requiring monitoring of drug levels in the blood). The doctors consulted with the clinical pharmacist in the department and decided to use a combination of piperacillin/tazobactam and amikacin (an aminoglycoside), monitoring kidney function and measuring drug levels in the blood to optimize treatment. As a result, Mr. N. showed significant improvement, his fever subsided, and he was weaned off the ventilator.
Nguyen Minh Tien (residing in District 8, Ho Chi Minh City), who frequently uses antibiotics for his children when the weather changes, said that while his family's medicine cabinet might be missing many other medicines, it's essential to have antibiotics like amoxicillin and penicillin on hand to prevent his children from catching colds during seasonal changes. Mr. Tien explained that his children often cough, and he's worried about the crowds at the hospital. He also mentioned that since his children's illnesses are mild and don't require hospitalization, he prefers antibiotics for convenience.
It's as easy as buying antibiotics in Vietnam.
According to Associate Professor Dr. Luong Ngoc Khue, Director of the Department of Medical Examination and Treatment Management ( Ministry of Health ), the invention of antibiotics is a miracle in modern medicine. The advent of antibiotics has greatly changed treatment methods, helping to eliminate dangerous bacteria, and thus many diseases have been controlled.
However, the reality of the past years shows that the irrational misuse of antibiotics by humans has created conditions for bacteria to develop resistance to antibiotics, rendering them virtually ineffective. It must be acknowledged that nowhere is it easier to buy antibiotics than in Vietnam – this is a major challenge for the community.
According to Professor Ngo Quy Chau, President of the Vietnam Respiratory Society and Director of Professional Services at Tam Anh General Hospital in Hanoi, the cause is the inappropriate use of antibiotics at all levels of the healthcare system, such as improper prescribing, poor hospital infection control, antibiotic use in aquaculture, livestock farming, and in the community... In particular, people's self-medication with antibiotics, arbitrarily increasing, decreasing, or skipping doses, also increases the risk of antibiotic resistance.
Statistics from Bach Mai Hospital (Hanoi) indicate that antibiotic resistance is increasing at an alarming rate year after year. In previous years, only a few cases of antibiotic resistance were reported at lower-level hospitals, but now, many patients transferred from lower-level facilities to Bach Mai Hospital have been found to have antibiotic-resistant bacteria upon initial bacterial culture. Many patients are admitted for other illnesses, but the infection escalates rapidly, and encountering antibiotic-resistant bacteria leads to critical conditions and death due to infection, not the underlying cause of admission.
 |
Risk of serious drug resistance
According to Dr. Le Quoc Hung, Head of the Department of Tropical Diseases at Cho Ray Hospital (Ho Chi Minh City), the use of antibiotics in Vietnam is currently quite indiscriminate. People can easily buy antibiotics at pharmacies, unlike in other countries where a doctor's prescription is required. Furthermore, in hospital settings, the rate of doctors using antibiotics is still very high, with nearly half of antibiotic prescriptions being inappropriate in terms of type, dosage, and timing.
Many antibiotic prescriptions are even "broadcasting," not to mention the misjudgment of the type of bacteria, which can sometimes lead to overuse of antibiotics and antibiotic resistance. "Many patients with antibiotic-resistant infections are very difficult to treat, resulting in long hospital stays, high antibiotic costs, and especially the need to use multiple antibiotics simultaneously to treat drug-resistant bacteria," Dr. Le Quoc Hung explained.
 |
| The doctor is advising the patient on how to use the medication safely. |
Commenting on the increasingly serious level of antibiotic resistance in Vietnam and the significant pressure it puts on public health, Mr. Cao Hung Thai, Deputy Director of the Department of Medical Examination and Treatment Management (Ministry of Health), stated that, in addition to the financial burden of prolonged treatment, we also face the possibility of a future without effective antibiotic treatments for some bacterial infections, especially for surgeries and treatments such as cancer chemotherapy and tissue transplantation.
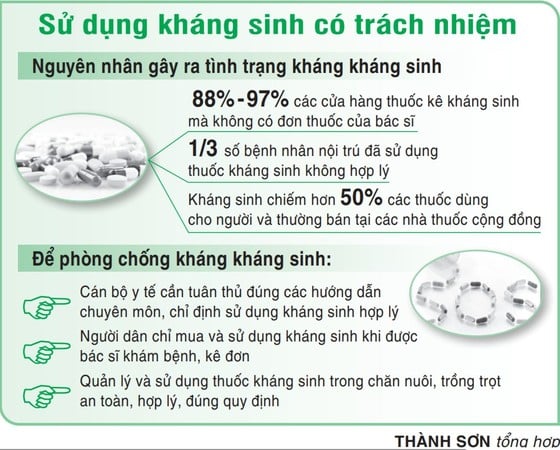
According to a survey by the health sector, the majority of antibiotics are sold without a doctor's prescription, reaching 88% in urban areas and 91% in rural areas. The problem of antibiotic resistance is becoming increasingly serious, with many bacteria resistant to multiple antibiotics, primarily due to antibiotic misuse. Most first and second-generation antibiotics currently available are ineffective. Hospitals are largely forced to use newer generation antibiotics in treatment.
The goal is to essentially control antimicrobial resistance by 2045.
Deputy Prime Minister Tran Hong Ha has just signed a decision approving the National Strategy on Antimicrobial Resistance Prevention and Control in Vietnam for the period 2023-2030, with a vision to 2045.
Specifically, from now until 2030, the strategy sets out four objectives: to raise awareness among local authorities and improve the understanding of healthcare workers, veterinarians, and the public about antimicrobial resistance prevention; to strengthen the antimicrobial resistance surveillance system to provide timely warnings about the emergence, spread, level, and trends of antimicrobial resistance in microorganisms; to reduce the spread of microorganisms and infectious diseases; and to use antimicrobial drugs in humans and animals rationally, safely, and responsibly.
The goal is to fundamentally control antimicrobial resistance by 2045, with an effective system for monitoring antibiotic resistance, use, and consumption.
According to experts, antibiotics are used to fight diseases in humans, animals, and plants, including antibacterial, antiviral, antifungal, and antiparasitic drugs. Antibiotic resistance occurs when bacteria, viruses, fungi, and parasites change over time and no longer respond to the drugs, making common infections more difficult to treat, increasing the risk of disease spread, severe illness, and death. The current state of antibiotic resistance is leading to an increasing number of infectious diseases (pneumonia, urinary tract infections, tuberculosis, etc.) becoming more difficult or even untreatable to treat.
Source



















































































































Comment (0)