Ho Chi Minh City The patient had a history of pancreatitis; recently had frequent abdominal pain and bloating; discovered a pancreatic cyst larger than 18 cm, milky white cyst fluid and a lot of necrotic tissue.
Mr. Ho Bac (44 years old, Thu Dau Mot City, Binh Duong ) has a history of necrotizing pancreatitis, which was treated two years ago but frequently recurred. He said that about a month ago, he had symptoms of abdominal pain, poor appetite, abdominal distension, and a large, hard mass. When he went to Tam Anh General Hospital in Ho Chi Minh City for examination at the end of May, Dr. Pham Huu Tung (Deputy Director of the Endoscopy and Endoscopic Surgery Center) noticed an abnormal mass protruding in the epigastric region (above the navel), and ordered tests and CT scans for diagnosis.
The results showed that the patient had a large epigastric cyst measuring 18.5x17 cm, occupying almost the entire epigastric region. The doctor suspected that this was a pancreatic pseudocyst due to complications of pancreatitis, causing a lot of fluid accumulation in this area. It was necessary to place a stent to drain the cyst into the stomach through endoscopic ultrasound.
Depending on the nature of the fluid assessed by endoscopic ultrasound (clear or thick, with a lot of necrotic tissue), the doctor will choose the appropriate drainage tube (plastic or metal tube). If the fluid is clear, the patient only needs to place a plastic drainage tube to drain effectively and at a low cost. If the fluid is thick, lumpy, and has a lot of necrotic tissue, a metal stent will be chosen and then the necrotic tissue will be removed endoscopically through the stent. Through endoscopic ultrasound, it is shown that the patient has lumpy cystic fluid and a lot of necrotic tissue inside, so a metal stent should be placed.
Dr. Huu Tung shared that in the past, treating pancreatic pseudocysts was a surgical or procedural intervention. Intervention with pancreatic pseudocysts is to drain the cyst, which is mostly drained into the intestine or stomach depending on the location of the cyst. However, nowadays, all are done by endoscopic surgery. With the advancement of gastrointestinal endoscopy, in cases where the cyst is located near the stomach - duodenum, it is possible to drain the cyst inward with a stent. The fluid from the cyst will be drained into the stomach and flow out through the digestive tract. This method is minimally invasive, safe and has few complications, leaving no scars for the patient.

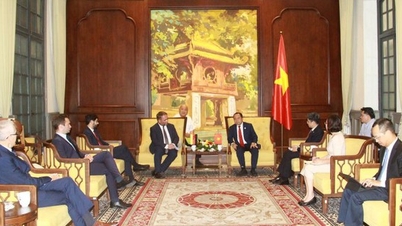
Doctor Huu Tung is analyzing the lesion in the pancreas through computed tomography (CT) scan. Photo: Provided by the hospital
After placing the metal stent, a lot of fluid flowed out, the doctor had to use an endoscope to suck out more than a liter of fluid, reduce the pressure on the cyst, reduce the risk of fluid reflux causing discomfort to the patient. However, there was still a lot of fluid and continued to flow through the stent into the stomach. The doctor took this fluid for biochemical testing to help diagnose the nature of the cyst. If it was a real cyst, it had to be cut off for thorough treatment. The patient's result was a pseudocyst of the pancreas.
The surgery lasted for one hour. Post-operatively, the patient's health was stable, no more pain or bloating, he was able to eat and drink again and was discharged the following day.

Mr. Bac no longer has bloating and abdominal pain after surgery. Photo: Provided by the hospital
Doctor Huu Tung said that pancreatic pseudocyst is a late complication of acute pancreatitis, chronic pancreatitis or pancreatic trauma. This is the result of inflammation and necrosis in the pancreas, manifested by abnormal fluid accumulation in the area around the pancreas, with a wall formed by fibrous tissue due to chronic inflammation. Acute pancreatitis or pancreatic trauma can lead to pancreatic pseudocyst after 4-6 weeks. Small pancreatic pseudocysts of 6 cm can heal on their own after conservative treatment, if larger than 6 cm have symptoms or complications, interventional treatment is required.
If large cysts are not treated, there is a risk of infection and abscess formation, pseudoaneurysm formation and hemorrhage or rupture, causing infection. When pancreatic fluid spills out, it can cause peritonitis, infection, and be life-threatening.
After surgery, patients should have a healthy lifestyle, limit alcohol, and have regular health check-ups to screen for possible recurrence of pancreatic pseudocysts.
Quyen Phan
Source link



![[Photo] Da Nang residents "hunt for photos" of big waves at the mouth of the Han River](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/10/21/1761043632309_ndo_br_11-jpg.webp)
![[Photo] Prime Minister Pham Minh Chinh meets with Speaker of the Hungarian National Assembly Kover Laszlo](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/10/20/1760970413415_dsc-8111-jpg.webp)
![[Photo] Prime Minister Pham Minh Chinh received Mr. Yamamoto Ichita, Governor of Gunma Province (Japan)](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/10/21/1761032833411_dsc-8867-jpg.webp)




































































































Comment (0)