Early detection of cancer is crucial for treatment and improving the chances of successful treatment. At this stage, doctors can intervene to reduce the risk of metastasis and increase the effectiveness of treatment, according to the health website Healthline (USA).

Mammograms can help detect early abnormalities of breast cancer.
There are many different cancer screening methods, ranging from imaging tests, blood tests, urine tests, cell tests, endoscopy, and several others. Much research evidence suggests that screening for cancer is the gold standard for early detection and treatment.
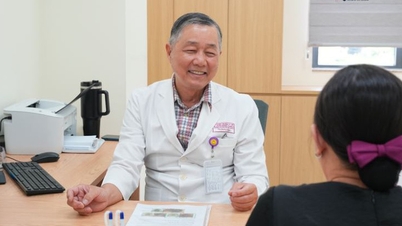
In women, breast and cervical cancer screening should begin at age 35. For breast cancer, women need to regularly check their breasts for any unusual lumps. At the hospital, doctors often screen for breast cancer using mammograms. Mammograms, or breast X-rays, help doctors detect abnormalities inside the breast.
Similarly, cervical cancer screening should begin at age 35. A PAP test, or cervical smear, will help detect precancerous and cancerous cells in the cervix.
Don't neglect colorectal cancer screening.
According to the U.S. Centers for Disease Control and Prevention (CDC), in addition to breast and cervical cancer, another type of cancer that can be effectively detected early through regular screening is colorectal cancer.
In most cases, colorectal cancer develops from precancerous polyps, which are lump-like lesions inside the colon or rectum. Screening can detect these precancerous lesions and remove them before they develop into cancer.
Lung cancer screening is often recommended for people at high risk. These include those with a history of heavy smoking, current smoking, those who have quit smoking within the past 15 years, and those aged between 50 and 80.
Cancers such as ovarian, pancreatic, prostate, testicular, bladder, oral, and skin cancer require screening for high-risk groups. These risk factors depend on sex, age, genes, weight, lifestyle, and several other factors, according to Healthline.
Source link






![[Photo] Prime Minister Pham Minh Chinh attends the Conference on the Implementation of Tasks for 2026 of the Industry and Trade Sector](/_next/image?url=https%3A%2F%2Fvphoto.vietnam.vn%2Fthumb%2F1200x675%2Fvietnam%2Fresource%2FIMAGE%2F2025%2F12%2F19%2F1766159500458_ndo_br_shared31-jpg.webp&w=3840&q=75)





































































































Comment (0)