
Patients will have their benefits reduced when they go to the wrong medical facility for examination and treatment (Illustration: Social Insurance of Ho Chi Minh City).
Mrs. Binh participates in health insurance with the initial medical examination and treatment registration place being the ward health station. Right in the ward where she lives, there is also a central hospital.
Ms. Binh asked: "To enjoy the right insurance coverage at the central hospital, do I still need a referral from the ward to the district and then to the central hospital? If I go directly to the central hospital for examination and treatment without using a referral, how much percentage will my health insurance card cover?"
According to Vietnam Social Security (VSS), referral of health insurance examination and treatment lines is regulated in Point a, Clause 1, Article 4, Circular No. 14/2014/TT-BYT of the Ministry of Health .
Accordingly, the transfer of patients from lower level to the next higher level is in the following order: level 4 transfers to level 3, level 3 transfers to level 2, level 2 transfers to level 1.
According to the Social Insurance, in the case of Ms. Binh registering for initial health insurance examination and treatment at the ward health station (level 4), in order to enjoy full health insurance benefits at the central hospital (level 1), she needs to have a referral letter in the above order.
Regarding the level of health insurance benefits when going to the wrong medical facility for examination and treatment, Vietnam Social Security said it is regulated in Clause 3, Article 22 of the 2008 Law on Health Insurance, amended in Clause 15, Article 1 of the Law on Amending and Supplementing a Number of Articles of the Law on Health Insurance.
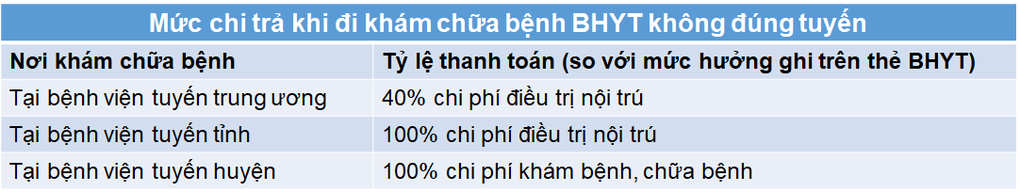
Based on the above regulations, if Ms. Binh goes to a central hospital for medical examination and treatment outside the prescribed medical facility and completes all required medical examination and treatment procedures under the Health Insurance Scheme (presenting her Health Insurance card and photo identification), she will be paid by the Health Insurance Fund at a lower level than the level she would have received if she had gone to a hospital for medical examination and treatment in accordance with the prescribed medical facility.
Specifically, Ms. Binh will be paid 40% of the inpatient treatment costs within the scope of payment of the health insurance fund and the benefit level stated on the card. In case Ms. Binh receives outpatient treatment, the health insurance fund will not pay.
In addition, because Ms. Binh went to the wrong medical facility for examination and treatment, her co-payment portion (if any) in the above case was not determined as a condition for granting a Certificate of Non-Co-Payment in the year.
Thus, Ms. Binh will not be entitled to 100% health insurance payment when the cost of health insurance examination and treatment in the year exceeds 6 months of basic salary (in case Ms. Binh has participated in health insurance for 5 consecutive years).
Source: https://dantri.com.vn/an-sinh/dung-the-bhyt-tuyen-phuong-len-trung-uong-chua-benh-duoc-chi-tra-bao-nhieu-20240523120412344.htm





![[Photo] Urgently help people soon have a place to live and stabilize their lives](/_next/image?url=https%3A%2F%2Fvphoto.vietnam.vn%2Fthumb%2F1200x675%2Fvietnam%2Fresource%2FIMAGE%2F2025%2F12%2F09%2F1765248230297_c-jpg.webp&w=3840&q=75)







































































![[Photo] General Secretary To Lam works with the Standing Committees of the 14th Party Congress Subcommittees](https://vphoto.vietnam.vn/thumb/402x226/vietnam/resource/IMAGE/2025/12/09/1765265023554_image.jpeg)

































Comment (0)