If detected and treated early in stages 1-2, lung cancer can be completely cured with a survival rate of up to 80% after 10 years.
Medical news January 21: High chance of survival when lung cancer is detected early
If detected and treated early in stages 1-2, lung cancer can be completely cured with a survival rate of up to 80% after 10 years.
80% 10-year survival rate in patients with early-stage lung cancer
In the online health consultation program with the topic "Minimally invasive thoracic surgery to treat early stage lung cancer" recently held, experts shared about minimally invasive surgical methods, especially the advantages of robotic surgery in treating early stage lung cancer.
 |
| Lung cancer is one of the dangerous diseases because it is difficult to detect in the early stages. |
According to Dr. Nguyen Huu Uoc, a reputable cardiovascular specialist, most lung cancer patients are diagnosed with the disease at stage 3 or 4. These are late stages where treatment is limited or impossible, and is mainly palliative.
Lung cancer is currently showing a tendency to become younger due to factors such as living environment, active and passive smoking, air pollution, and especially gene mutations that increase the risk of cancer. Therefore, methods for early diagnosis of lung cancer are gradually being developed, in which gene mutation detection techniques play an important role.
According to Dr. Nguyen Huu Uoc, most patients proactively come for examination, which results in a higher rate of early detection of the disease. The hospital continuously invests in and develops new techniques for early diagnosis of lung cancer and other types of cancer, while also proposing timely and effective treatment solutions.
Lung cancer is one of the dangerous diseases because it is difficult to detect in the early stages. The signs of lung cancer are often easily confused with other diseases such as sore throat, respiratory tract infection, or cardiovascular problems.
Common symptoms are prolonged cough, sore throat, respiratory tract infection. Chest pain (due to tumor compression), pain behind the shoulder, back pain. Hoarseness, hoarseness. Coughing up blood, wheezing. Shoulder and muscle pain.
Doctors recommend that people with risk factors should screen for lung cancer early, especially those over 50 years old, smoke heavily, work in toxic environments, are exposed to radiation or have underlying medical conditions.
With the development of minimally invasive surgery, thoracoscopic surgery is now widely used in the treatment of early stage lung cancer.
This technique helps detect small lesions, thereby effectively treating them. Post-operative patients will be closely monitored and have regular CT scans performed in 1, 3, 6 months and 1 year. If there are no signs of recurrence, the patient will be assessed as cured after 2-5 years.
With early diagnosis and minimally invasive surgery, the success rate in treating early stage lung cancer can be up to 90%. Therefore, experts encourage patients to visit and treat early for the best results.
Currently, the latest generation Davinci XI Robot system allows doctors to perform complex surgeries with high precision, superior safety and faster recovery time.
About endoscopic surgery for early stage lung cancer. This is a popular surgical method in the world and is also widely applied in Vietnam today.
Robotic surgery helps the surgeon control the robotic arms, minimizing vibration or fatigue of the surgeon. The 3D camera system helps to clearly observe the anatomical structure during surgery, thereby increasing accuracy and reducing the risk of complications.
Detecting late stage colon cancer through symptoms of prolonged fatigue
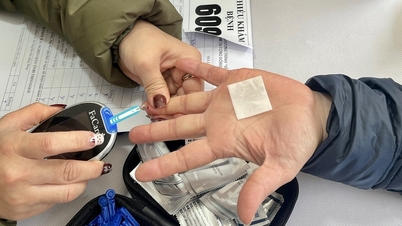
Ms. L., 65 years old, a healthy woman, but recently began to feel persistent fatigue and palpitations after eating. These symptoms are not very obvious and can easily be confused with common digestive problems.
When this condition did not improve, Ms. L. decided to go for a general health check-up. The results of the examination and tests at Tam Anh Clinic in District 7 surprised her when they discovered stage 3B colon cancer, with cancer cells that had metastasized to the lymph nodes.
According to Master, Doctor Ngo Hoang Kien Tam, a digestive endoscopy specialist, although the patient did not have typical symptoms such as fever or weight loss, severe anemia and prolonged fatigue are important signs to detect colon cancer.
Ms. Lan's blood test results showed that her hemoglobin index had dropped to 7.0 g/dl, while the normal index for women ranges from 12 to 16 g/dl. This anemia made her feel tired and lifeless.
In addition, abdominal computed tomography (CT) scan results showed signs of colon wall thickening, loss of transverse colon structure at the hepatic flexure, fatty infiltration, and small surrounding lymph nodes.
Through colonoscopy, the doctor discovered a polyp in the hepatic flexure of the colon with an ulcerated surface that bleeds easily.
After performing a polypectomy and biopsy, the results showed that the polyp in the hepatic flexure was a moderately differentiated tubular adenocarcinoma, invading the outermost layer of the colon, while the low-grade hyperplastic polyp was benign. High-grade dysplasia is considered a precancerous tumor, with the potential to turn into cancer if not treated promptly.
The pathology results showed stage 3B colon cancer with one metastatic lymph node out of 14 lymph nodes sampled. This is one of the reasons why late stage colon cancer has a low survival rate, but if detected early, the chance of a complete cure can be up to 95%.
After her health stabilized, Ms. L. was assigned to undergo laparoscopic surgery to resect the right colon and dissect the lymph nodes. The surgery was performed with the support of 3D/4K ICG Rubina Karl Storz laparoscopic surgery technology, helping the doctor observe more clearly and accurately during the surgery. At the same time, the use of ICG (Indocyanine Green) dye helps to check the blood supply at the anastomosis, minimizing the risk of anastomosis leakage after surgery.
Colon cancer is one of the most common malignancies of the digestive tract and is the third leading cause of cancer death.
In Vietnam, the number of colon cancer cases is on the rise, especially in people with unscientific diets, little exercise or smoking habits.
Early stage colon cancer has few obvious symptoms, so early detection is often difficult. Signs of the disease, such as bloody stools, changes in bowel habits, changes in stool shape, abdominal pain, tenesmus, or anemia can easily be confused with common digestive diseases.
Bleeding and blood loss are common symptoms in patients with advanced colon cancer, and in Ms. Lan's case, this condition had been simmering for a long time without being detected until she felt tired and weak. If the disease is not detected in time, dangerous complications such as intestinal obstruction or gastrointestinal bleeding can occur.
To prevent colon cancer, Dr. Tam recommends that people should build a healthy lifestyle, minimize risk factors, and especially have regular health check-ups and perform screening tests such as colonoscopy to detect the disease early. Early detection of colon cancer can help treat it effectively, reduce mortality and give patients a chance of long-term survival.
Thought bronchitis turned into serious heart disease
Mr. T., 35 years old, had been suffering from a persistent fever, severe cough and difficulty breathing for a month. At first, he thought he had bronchitis and bought medicine to take himself.
However, his cough, fatigue and difficulty breathing became more severe, causing him to lose 3.5 kg. Although he was treated for bronchitis at a medical facility, the symptoms did not improve, forcing him to go to a specialized medical facility for examination.
Here, the doctors discovered a much more serious problem. The examination results showed that Mr. T's four heart chambers were very dilated, along with a calcified mass measuring 13x5 mm in the aortic valve ring. In addition, the right coronary sinus - a part of the aortic root - was enlarged and ruptured, causing moderate aortic valve regurgitation.
Mr. T. shared that since birth, he had a congenital heart defect: infundibular ventricular septal defect. This is a congenital heart defect that causes a hole between the two ventricles, located just below the pulmonary valve on the right ventricle. At that time, oxygen-rich blood from the left ventricle will pass through the hole and mix with oxygen-poor blood in the right ventricle.
According to the treating physician, the patient did not follow up and return for a check-up for more than ten years, causing the initial ventricular septal defect to progress, leading to complications of rupture of the right coronary sinus, and eventually causing severe heart failure.
This complication has become rare in recent times because most cases of ventricular septal defect are detected and treated early. The doctor also said that a common cause of rupture of the right coronary sinus aneurysm is infective endocarditis, so careful screening and evaluation of the patient's condition is very important.
The doctors performed surgery to remove the calcified mass at the edge of the ventricular septal defect, cut and reconstructed the ruptured right coronary sinus aneurysm, and repaired the aortic valve. Compared with valve replacement, aortic valve repair surgery is much more difficult. The surgeon needs to have a clear understanding of the three-dimensional anatomical structure in this area.
After surgery, Mr. T.'s cardiac contractility and heart failure improved significantly. He was treated with low-dose vasopressors, the aortic valve functioned well, the hole was closed, the right coronary sinus was well formed, and there were no surgical complications. The patient was discharged and asked to return for regular check-ups to monitor his health.
Infundibular ventricular septal defect is a rare type of congenital heart defect, accounting for about 5-7% of ventricular septal defect cases. If the defect is small and does not affect neighboring structures, as well as having no complications, then surgery is not required because the defect can close on its own as the patient grows up. However, the patient still needs to be monitored periodically to detect any symptoms.
When the ventricular septal defect is of medium size or larger, accompanied by cardiac chamber dilation, pulmonary hypertension in children or progressive aortic valve regurgitation in adults, the patient needs surgery.
If not properly monitored and treated, the disease can progress, causing dangerous complications such as heart failure, pulmonary hypertension, infective endocarditis, arrhythmias and valvular heart disease.
Source: https://baodautu.vn/tin-moi-y-te-ngay-211-co-hoi-song-cao-khi-phat-hien-ung-thu-phoi-som-d241594.html




![[Photo] The Standing Committee of the Organizing Subcommittee serving the 14th National Party Congress meets on information and propaganda work for the Congress.](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/11/19/1763531906775_tieu-ban-phuc-vu-dh-19-11-9302-614-jpg.webp)




























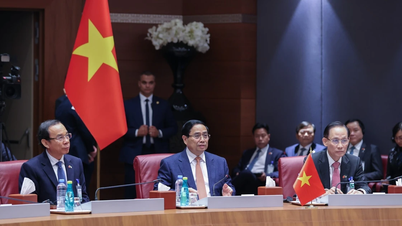
![[Photo] Prime Minister Pham Minh Chinh and his wife meet the Vietnamese community in Algeria](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/11/19/1763510299099_1763510015166-jpg.webp)








































































Comment (0)