Currently, there is no specific treatment for measles, so vaccination is the most effective preventive measure.
Latest news on March 21: Ministry of Health issues 10 messages on measles prevention
Currently, there is no specific treatment for measles, so vaccination is the most effective preventive measure.
According to the Ministry of Health , measles is one of the leading causes of death in children due to serious complications such as pneumonia, encephalitis, severe diarrhea and malnutrition.
Ministry of Health warns about measles situation in children
Statistics from the Ministry of Health show that since the beginning of 2025, the country has recorded about 40,000 suspected cases of measles, including 5 deaths related to the disease. Measles cases are mainly concentrated in the South (57%), Central (19.2%), North (15.1%) and Central Highlands (8.7%).
 |
| Measles is one of the leading causes of death in children due to serious complications such as pneumonia, encephalitis, severe diarrhea and malnutrition. |
At the recent national online conference on measles prevention and control, Minister of Health Dao Hong Lan warned about the complicated epidemic situation.
Although measles is a vaccine-preventable disease, the number of cases is still increasing in many countries, including Vietnam. Minister Dao Hong Lan emphasized that measles epidemics may continue to increase in the coming time, especially in high-risk areas such as mountainous provinces, ethnic minority areas and areas with low vaccination rates.
In the face of the complicated developments of the epidemic, Minister Dao Hong Lan requested the People's Committees of provinces and cities to prioritize resources to speed up the progress of the measles vaccination campaign. Priority subjects are children who are not yet old enough to be vaccinated or have not received enough doses of vaccine. The Ministry of Health requires the vaccination campaign to be completed by March 2025.
The Minister also called on localities to strengthen communication and mobilize people to fully vaccinate and proactively prevent measles. At the same time, provinces and cities need to review and vaccinate areas with low vaccination rates to prevent the disease from spreading. Medical facilities need to prepare medical supplies and reserve drugs to prevent cross-infection in medical facilities.
Implementing the Prime Minister 's direction in Official Dispatch No. 23/CD-TTg dated March 15, 2025, the Ministry of Health has compiled the vaccine needs of localities and developed a plan for the second phase of measles vaccination in 2025. Up to now, 63/63 provinces and cities have been implementing catch-up and catch-up vaccination campaigns for subjects who have not received enough doses.
To support the campaign, the Ministry of Health has mobilized aid from VNVC with 500,000 doses of measles vaccine. In addition, 500,000 doses of measles vaccine will be used to catch up on vaccinations for children aged 1-5 who have not received enough doses of vaccine under the Expanded Immunization Program.
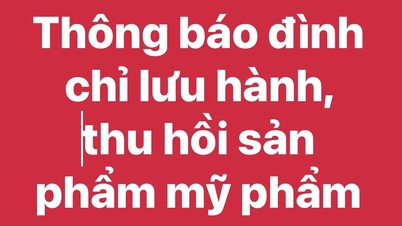
To prevent the epidemic, the Ministry of Health issued 10 important messages as follows: Measles spreads quickly and can easily cause an epidemic.
When a child has measles or is suspected of having measles, isolation is needed to avoid infection. Measles is one of the leading causes of death in children due to dangerous complications.
Measles vaccination is the most effective preventive measure, as there is no specific treatment for measles. Children should receive the first dose of measles vaccine at 9 months of age and the second dose at 18 months of age according to the Expanded Immunization Program.
The measles vaccination campaign for children aged 6-9 months and 1-10 years aims to prevent the disease and its serious complications. Children who have not received or have not received two doses of the vaccine should be vaccinated during the vaccination campaign.
Parents should take their children to vaccination points to participate in the measles vaccination campaign. The measles vaccine is safe and effective, and may cause mild reactions such as fever or rash, which will go away after a few days. If your child has a high fever, persistent crying, difficulty breathing or poor feeding after vaccination, take him or her to a medical facility.
Millions of Vietnamese people have hepatitis without knowing it.
Hepatitis B and C, if not treated promptly, can silently progress to cirrhosis, liver cancer, and is the cause of death for millions of people. However, many Vietnamese people still do not realize they have the disease and have not received proper treatment.
It is estimated that Vietnam has about 7.6 million people infected with the hepatitis B virus, but only more than 1.6 million have been diagnosed and about 45,000 have received treatment.
Similarly, only about 60,000 people are diagnosed with hepatitis C, while nearly one million are actually infected. Vietnam is currently among the top 10 countries with the highest rates of hepatitis B and C infection in the world. In addition, about 40 million Vietnamese people are not immune or have not been vaccinated against hepatitis B.
Chronic hepatitis B and C are the main causes of about 80% of liver cancer cases, a disease that is on the rise. This type of cancer has a poor prognosis, low survival rate and is the leading cause of death, with more than 23,000 cases each year in Vietnam, according to data from the International Agency for Research on Cancer (Globocan).
Associate Professor, Dr. Bui Huu Hoang, Vice President of the Ho Chi Minh City Medical Association and President of the Ho Chi Minh City Liver and Bile Association, warned that chronic hepatitis B and C develop silently, gradually damaging the liver and can lead to cirrhosis or liver cancer if not detected and treated promptly.
Of the deaths from liver cancer, more than 50% are due to hepatitis B virus, and 26% are due to hepatitis C. Unfortunately, most patients only discover the disease at a late stage, when effective treatment is no longer possible. It is predicted that the incidence of cirrhosis and liver cancer will continue to increase if there is no expansion in diagnosis and treatment.
Associate Professor Hoang recommends that testing for viral hepatitis can save lives and is an important first step in preventing infection.
Vietnam is aiming to eliminate hepatitis by 2030, but the biggest challenge now is that the rate of people aware of their infection status is still too low.
A 2024 survey found that about 66% of respondents thought that testing for hepatitis B and C was not important and that they felt their health was fine. Previously, a survey by the Ministry of Health also found that more than 52% of people had never heard of hepatitis B and C.
In addition to low awareness, treatment costs and lack of screening programs for viral hepatitis are also major barriers. According to Dr. Nguyen Bao Toan, Head of the Laboratory Department, Ho Chi Minh City Medic Center, currently, screening for hepatitis B through HBsAg testing is still not enough to assess the infection status.
Some people have been infected with the virus for a long time, the antigen concentration decreases, making the test unable to detect. Therefore, additional tests such as the HBsAg, Anti-HBc, Anti-HBs trio are needed for more accurate results. However, many medical facilities have not yet deployed this technique.
The cost of treating hepatitis is still high. Hepatitis B patients need to spend about 80,000-1,300,000 VND/month and must be treated for life.
Hepatitis C treatment costs about 20-21 million VND for 12 weeks of treatment, while insurance only covers 50%. In addition, international aid programs are decreasing, greatly affecting disease prevention work.
According to the Ministry of Health's 2019 guidelines, pregnant women must be screened for hepatitis B infection during their first prenatal visit, along with HIV and syphilis. However, currently only about 60-70% of pregnant women are screened for hepatitis B nationwide. In particular, there is still no data on pre-pregnancy screening, an important time for treatment to prevent mother-to-child transmission of HBV.
Detecting congenital heart disease from high blood pressure symptoms
Mr. Tan, 31 years old, suddenly discovered that he had aortic stenosis after his blood pressure remained high despite taking medication regularly for three months.
Before that, he always felt healthy, had no problems with his daily activities and work, and only occasionally felt slightly dizzy.
However, when measuring his blood pressure, he discovered that his blood pressure ranged from 180-200 mmHg and started taking blood pressure medication, but his condition did not improve, his blood pressure remained at 160-180 mmHg.
On March 21, Dr. Pham Thuc Minh Thuy, Department of Congenital Heart Disease, Cardiovascular Center, Tam Anh General Hospital, Ho Chi Minh City, said that Mr. Tan's son, now 5 years old, had undergone surgery to repair aortic coarctation when he was just over 1 year old.
Coarctation of the aorta is a congenital heart disease and is currently being monitored at Tam Anh General Hospital. During the examination and consultation with the family, the doctor explained the condition of Mr. Tan's son and advised him and his wife to have a heart check.
When Mr. Tan and his wife arrived at the hospital, Dr. Thuy noticed that Mr. Tan's blood pressure was very high, especially with a clear difference between blood pressure in his arms and legs (blood pressure in his arms was about 200 mmHg, while blood pressure in his legs was only about 120 mmHg).
Suspecting that Mr. Tan had aortic stenosis like his son, the doctor asked him to do an echocardiogram. The results surprised him when he discovered he had this congenital heart disease at the age of 31.
This is a special case, like “giving birth to the child before giving birth to the father”, meaning the parents do not know about their illness until it is accidentally discovered during the treatment of their child.
Coarctation of the aorta is a narrowing of the aorta, causing reduced blood flow through that artery. Over time, this can alter the carotid baroreceptors and reduce blood flow to the kidneys, activating the renin-angiotensin-aldosterone system, causing high blood pressure.
Mr. Tan's case was also accompanied by a bicuspid aortic valve disease (instead of the normal tricuspid), leading to abnormal opening and closing of the valve, causing aortic valve regurgitation. This, together with abnormal vortex blood flow, caused dilation of the sinus of Valsalva and dilation of the ascending aorta.
Mr. Tan was asked to do additional paraclinical tests to check for other abnormalities such as kidney cysts (abdominal ultrasound showed no problems with his kidneys) and cerebral aneurysms (fortunately, the brain MRI results did not show any aneurysms).
Mr. Tan's aortic stenosis has progressed, causing increased pressure in the artery in front of the stenosis, resulting in left ventricular hypertrophy and increased blood pressure in the upper limbs. This also prevents his blood pressure from decreasing despite medication.
Dr. Vu Nang Phuc, Head of the Congenital Heart Department, said that Mr. Tan's condition was very dangerous, especially when the aortic coarctation tightened, causing great pressure on the left ventricle. If not intervened promptly, the disease could cause serious complications such as chronic hypertension, cerebral hemorrhage, aortic aneurysm, heart failure, kidney failure, and even death.
The doctor ordered Mr. Tan to have a CT scan of the aorta to determine the size, location, and length of the narrowed artery segment, as well as to assess the calcification around the narrowed area, because calcification can pose a risk of aortic rupture during intervention.
The results showed that the medical team chose a stent with an outer membrane with a diameter of 16 mm, suitable for the size of the artery.
The intervention was successful, the doctor used a balloon-attached stent to dilate the aorta at the narrowed position.
After the stent was placed in the correct position, the doctor performed a balloon dilation to expand the stent, hugging the aortic wall. After the procedure, Mr. Tan's blood pressure dropped to 130/80 mmHg, and the blood pressure index between the upper and lower limbs was similar. He was discharged from the hospital just two days later.
Dr. Phuc confirmed that aortic stenosis can be treated, but patients need to be monitored long-term. After intervention, patients still have the risk of re-stenosis, aortic aneurysm, or still have high blood pressure.
In particular, patients need to develop a scientific diet, exercise regularly and have regular check-ups. Women who have been treated for aortic stenosis and intend to become pregnant should discuss carefully with their doctor before making a decision.
Aortic coarctation has many potential dangerous complications and is often detected late due to the lack of obvious symptoms.
Some patients may exhibit symptoms such as pale skin, excessive sweating, rapid breathing, labored breathing, rapid pulse, poor feeding (in children); headache, high blood pressure, kidney problems, leg weakness during physical activity (in adults).
Therefore, if there are any unusual symptoms or a family history of cardiovascular disease, patients need to see a doctor immediately for timely treatment and to limit dangerous complications.
Source: https://baodautu.vn/tin-moi-ngay-213-bo-y-te-dua-ra-10-thong-diep-phong-chong-dich-soi-d257050.html




![[Photo] Opening of the 14th Conference of the 13th Party Central Committee](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/11/05/1762310995216_a5-bnd-5742-5255-jpg.webp)
























![[Photo] Panorama of the Patriotic Emulation Congress of Nhan Dan Newspaper for the period 2025-2030](https://vphoto.vietnam.vn/thumb/1200x675/vietnam/resource/IMAGE/2025/11/04/1762252775462_ndo_br_dhthiduayeuncbaond-6125-jpg.webp)






































































Comment (0)